Torticollis, often referred to as “twisted neck” or “wry neck” is a condition that leads to an abnormal, asymmetrical head or neck position, which can cause significant discomfort and neck pain. This blog explores the symptoms, causes, treatments, and preventive measures for torticollis in adults, with a special emphasis on the role of neck pain physical therapy. Understanding these elements can help patients manage and treat their conditions effectively.
What is Torticollis?
Torticollis is a condition in which patients keep their head tilted to one side, often away from the affected side. Torticollis has various causes, ranging from congenital structural abnormalities to acquired muscle or nerve dysfunction. In adults, torticollis can particularly impact daily activities and contribute to ongoing neck pain.
Symptoms of Torticollis in Adults
The primary symptom of torticollis is an obvious and abnormal positioning of the head. However, several other symptoms can accompany this condition:
- Persistent pain and discomfort in the neck
- Stiffness of the neck muscles
- The head and neck have a limited range of motion
- Headache and dizziness
- Swelling or thickening of the neck muscles
Causes of Torticollis in Adults
Torticollis, a complex condition affecting the neck muscles, has two types: congenital and acquired. Each type has distinct origins and mechanisms, which are essential to understanding for effective management and treatment.
Congenital Torticollis
Congenital torticollis, also known as “infantile torticollis,” appears in infants often due to positioning in the womb or complications during birth that affect muscle development in the neck. Here are some detailed factors contributing to congenital torticollis:
Intrauterine Malposition: Limited space in the womb can force the foetus into an awkward position, causing excessive pressure on the neck muscles, particularly the sternocleidomastoid muscle, which can lead to its shortening.
Fibrosis of the Sternocleidomastoid Muscle: This is the most common cause of congenital torticollis. The muscle may sustain damage, resulting in scar tissue, which shortens and tightens the muscle, pulling the head towards the affected side.
Birth Trauma: Difficult births, especially those requiring interventions like forceps or vacuum extraction, can lead to muscle or nerve damage in the neck of the newborn.
Genetic Factors: While less common, there can be genetic influences that predispose infants to muscle abnormalities that lead to torticollis.
These factors often require early intervention, typically involving gentle stretching exercises, physical therapy for neck pain, and, in some rare cases, surgical procedures to release tight muscles.
Acquired Torticollis in Adults
Image Source: Motivationaldoc
Acquired torticollis occurs later in life and can be triggered by several different factors, which can vary greatly in severity:
Trauma: Sudden head or neck injuries, such as those from car accidents or falls, can damage the cervical spine and associated muscles, leading to torticollis. Such trauma can induce inflammation or direct injury to the neck muscles or ligaments.
Adverse Reactions to Medications: Certain medications, particularly those that affect neurotransmitter levels like dopamine, can cause dystonic reactions. These reactions can lead to abnormal neck postures, a condition often referred to as drug-induced torticollis.
Infections: Bacterial or viral infections can involve the neck’s lymph nodes, muscles, or vertebrae. An example is a retropharyngeal abscess, which can cause the neck muscles to spasm and tilt the head.
Neurological Disorders: Conditions affecting the brain, spinal cord, or nerves, such as cervical dystonia or Parkinson’s disease, can cause persistent muscle contractions leading to chronic torticollis.
Degenerative Spinal Diseases: Diseases like cervical disc degeneration or arthritis can indirectly lead to torticollis due to the uneven stress on neck muscles as the body tries to compensate for the pain or structural changes in the spine.
Managing acquired torticollis involves treating the underlying cause, which may include medications to reduce inflammation, pain, and muscle spasms, and physical therapy for neck pain to restore mobility and strengthen muscles. At times, physical therapy helps to avoid surgery altogether.
Understanding the specific causes and mechanisms of torticollis is crucial for diagnosing and devising effective treatment plans. Although arising from different origins, both types of torticollis significantly impact the affected individual’s quality of life and, as such, require tailored approaches in management and intervention.
Torticollis Treatment in Adults
Twisted neck treatment options vary based on the severity and underlying cause of torticollis but typically include the following approaches:
Medication
Nonsteroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants can help reduce pain and muscle activity.
Physical Therapy
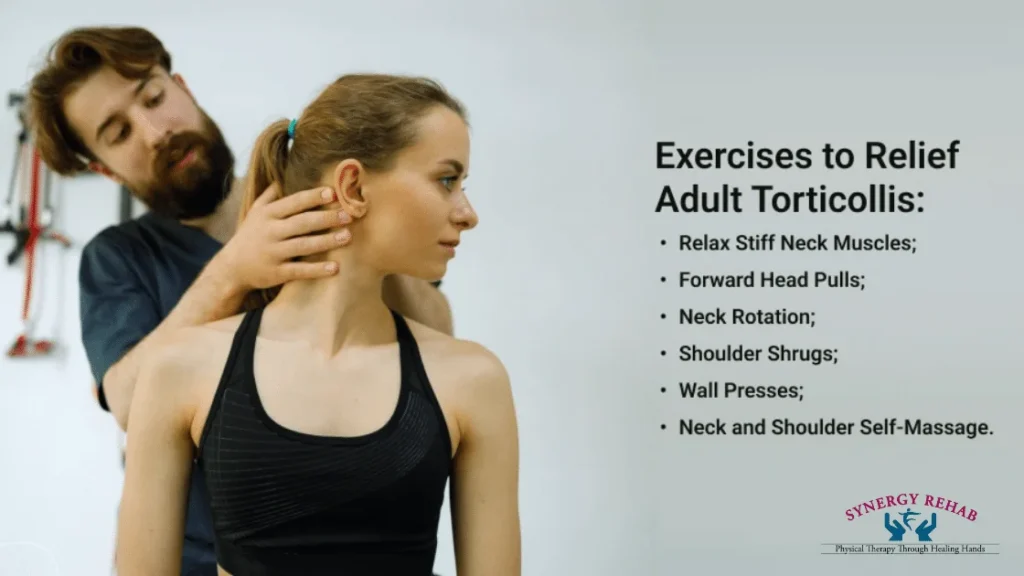
Physical therapy is a cornerstone of treatment for torticollis in adults and is particularly effective in managing neck pain. Therapists may employ techniques such as:
- Stretching exercises to improve flexibility and range of motion.
- Strengthening exercises to support neck muscles.
- Manual therapy to reduce muscle tightness and pain.
- Postural training to correct alignment and prevent recurrence.
Role of Physical Therapy in Managing Torticollis
Physical therapy plays a pivotal role in the treatment of torticollis by addressing the direct symptoms and underlying causes of the condition. A tailored physical therapy for neck pain program can offer several benefits:
Alleviation of Pain and Discomfort: Through therapeutic exercises and modalities such as heat or ice applications, TENS (transcutaneous electrical nerve stimulation), and ultrasound therapy.
Improvement in Mobility: Stretching and strengthening exercises enhance the range of motion and strength of neck muscles.
Correction of Postural Issues: Educating patients on proper posture to reduce stress on the cervical spine.
Physical therapy strengthens neck muscles and improves flexibility, helping to treat existing symptoms and prevent the recurrence of torticollis.
Prevention of Torticollis
Preventing torticollis primarily involves maintaining good neck health and posture. Regular exercise, ergonomic adjustments in the workplace, and being mindful of neck positions during daily activities can significantly reduce the risk. Additionally, treating any minor neck injuries promptly and effectively can prevent them from developing into more severe conditions.
Final Thoughts
While potentially debilitating, torticollis can be effectively managed with the right combination of twisted neck treatment through physical therapy. If you’re experiencing symptoms of torticollis, such as persistent neck pain or abnormal head posture, it’s crucial to seek professional medical advice.
This detailed exploration of torticollis should empower individuals suffering from this condition with the knowledge they need to seek effective treatment and manage their symptoms proficiently.
At Synergy Rehab, we specialize in neck pain physical therapy and treating conditions like torticollis. Our team of experienced physical therapists is dedicated to providing personalized care to help you regain comfort and functionality. Don’t let neck pain hold you back. Contact Synergy Rehab today and take the first step towards a pain-free life!
FAQs on Physical Therapy for Torticollis
Q1. What specific physical therapy techniques are used to treat torticollis?
Physical therapists use various techniques to treat torticollis, including manual therapy to manipulate and mobilize muscles and joints, targeted stretching exercises to alleviate tightness, and strengthening exercises to support the neck. Modalities such as ultrasound or electrical stimulation may also reduce pain and inflammation.
Q2. How long does it take for physical therapy to improve torticollis?
The duration of physical therapy for torticollis depends on the severity and type of the condition. Most patients see improvement within several weeks, but it can take several months of consistent therapy to achieve optimal results. Progress is usually gradual and depends on patient compliance with therapy both in sessions and at home.
Q3. Can physical therapy completely cure torticollis?
Physical therapy can significantly improve the symptoms of torticollis and, in many cases, can lead to a complete resolution, especially in acquired instances where the condition is caused by temporary factors such as muscle strain or injury. However, while symptoms can be greatly improved in congenital cases, some residual effects may persist.
Q4. Are there any risks associated with physical therapy for torticollis?
Physical therapy for torticollis is generally safe when performed by a licensed and experienced therapist. However, as with any treatment, there are some risks, such as muscle soreness and fatigue following treatment. Rarely, improper techniques can lead to increased pain or injury, underscoring the importance of working with a qualified professional.
Q5. What should I expect during my first physical therapy session for torticollis?
During your first session, the physical therapist will conduct a thorough assessment, which includes a medical history review and a physical examination of your neck’s range of motion, muscle strength, and posture. This initial evaluation helps to create a customized treatment plan. You may also receive education about your condition and some initial treatment during your first visit.